


COVID-19 Doctor Wellbeing Study

Source: Simon Davis/DF»
Scottish Medical Education Research Consortium (SMERC) COVID-19 Research Study
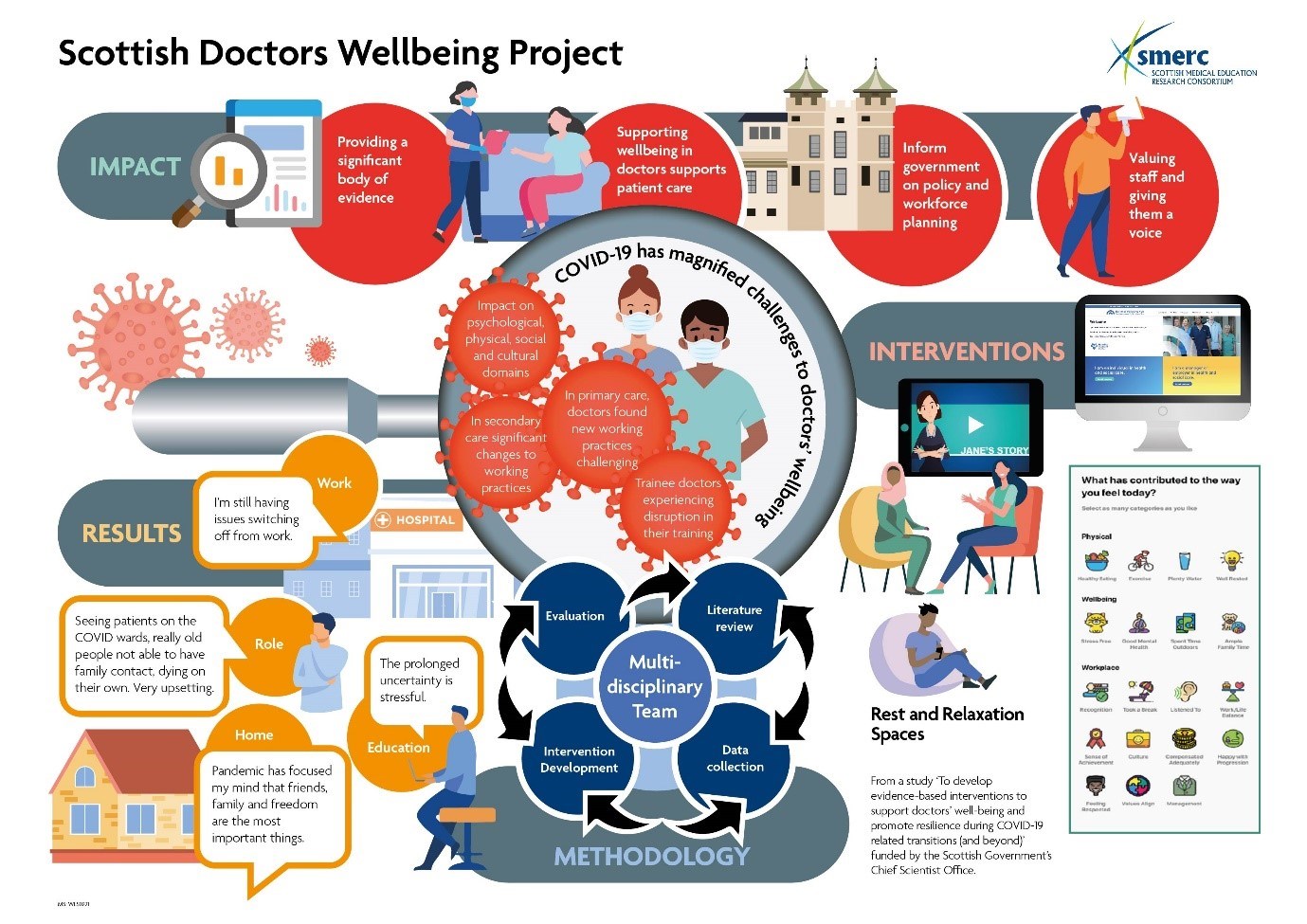
SMERC is currently involved in a COVID-19 research study which aims to develop evidence-based interventions to support doctors’ wellbeing and promote resilience during COVID-19 related transitions (and beyond). The research is a collaboration between medical schools at the Universities of Aberdeen, Dundee, Edinburgh, Glasgow, and St Andrews and NHS Education for Scotland (NES) and was funded initially by the Scottish Government through the Chief Scientists Office (CSO) and more latterly from SMERC research funds for the main project.
» CSO Project Map (pptx)

Research team
Kim Walker, Katie Gibson Smith (University of Aberdeen), Lisi Gordon, Gillian Scanlan (University of Dundee), Gill Aitken (University of Edinburgh), Lindsey Pope (University of Glasgow), Jo Cecil, Anita Laidlaw, Patrick Cairns, Kathryn Cunningham, Tricia Tooman (University of St Andrews), Peter Johnston, Julie Ferguson, Judy Wakeling (NHS Education for Scotland).
Dissemination of results
The initial results from the project have been disseminated in several ways and across many different platforms.
The initial report provided to the CSO can be accessed here: CSO Report
We have also produced an infographic:
A knowledge exchange workshop was held on 8th September between the project team, Scottish Government representatives and NHS representatives. The initial presentation can be seen here: Knowledge Exchange Workshop
The team have presented on various aspects of the project at many local, national and international conferences. These include: NHS Education Days, Association for the Study of Medical Education (ASME) ASM, Association for the study of Medical Education in Europe (AMEE) annual meeting, Scottish Medical Education Conference (SMEC) annual meeting, NHS Employers, and Royal College of General Practitioners.
What we have done
The study used a pragmatic rapid research design underpinned by a theoretical framework. Work is still ongoing to analyse all the data. However, preliminary results are available. The interventions are in various stages of implementation and evaluation.
Further information on the various stages including publications can be found below.
Workstream 1 - a scoping review of the literature
Previous research has revealed the negative effect of pandemics on healthcare workers wellbeing, including increased exposure to harm, vulnerability, uncertainty, anxiety, distress, depression and disrupted sleep. The purpose of this scoping review was to search for pre-existing interventions to support doctors during pandemics. As the review progressed, it became evident that the existing literature relating to interventions for doctors during pandemics either didn’t exist or was very small. It was therefore decided to broaden the study population to Health care workers and look beyond pandemics to other crises including natural disasters.
The academic literature contains no interventions for the wellbeing of doctors during a pandemic. 13 interventions were found relating to interventions for the wellbeing of HCWs during a crisis. These were prospective and descriptive studies. These were judged to be of poor quality and not appropriate to base intervention development upon.
This work has been written up and published.
Cairns P, Aitken G, Pope L, Cecil J, Cunningham K, Ferguson J, Gibson Smith K, Gordon L, Johnston P, Laidlaw A, Scanlan G, Tooman T, Wakeling J & Walker K (2021) Interventions for the well-being of healthcare workers during a pandemic or other crisis: a scoping review. BMJ Open 10.11.36/bmjopen – 2020-047498
Workstream 2 – data collection
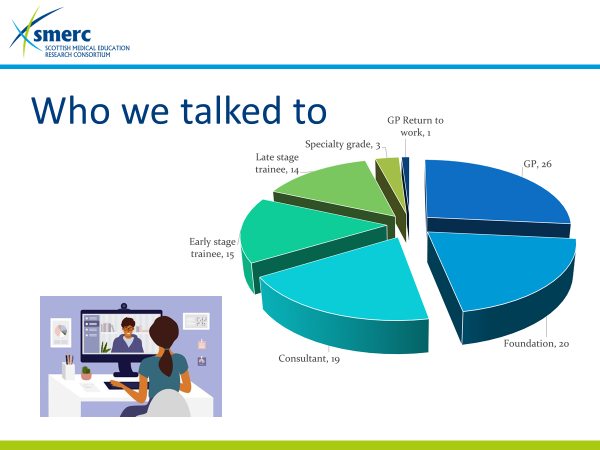
We have recruited over 120 doctors and in total, we have interviewed 100 people across all grades: FiY: Foundation Doctors: Trainees at all levels; Consultants; GP’s and Retired/returning doctors. The participants represent every Health Board in Scotland and have a geographical diversity. A major achievement. In addition, as part of our longitudinal study, 66 participants have provided audio-diaries since July. A significant amount of data. 83 participants undertook a 2nd interview.
Initial coding and analysis of the transcripts has been done. We have identified key areas relating to doctors’ wellbeing and resilience during COVID-19-related transitions and beyond. As the pandemic seems to be continuing and with the advent of winter pressures, the “and beyond” will become even more important.
The initial work has been analysed and is now published in Medical Education.
Lisi Gordon, Gillian M. Scanlan, Tricia R. Tooman, Kim A. Walker, Patrick Cairns, Julie Ferguson, Gillian Aitken, Joanne Cecil, Kathryn B. Cunningham, Kathrine Gibson Smith, Peter W. Johnston, Anita Laidlaw, Lindsey M. Pope, Judy Wakeling. Heard, valued, supported? Doctors' wellbeing during transitions triggered by COVID-19. Med Educ. 2021. https://doi.org/10.1111/medu.14698
Workstream 3 – intervention development and intervention
The key themes for this study are considering the psychological, physical, social and cultural domains. As this project has a short timeline, we could only consider a few interventions – we had many more ideas! To help with our prioritisation, we conducted two expert panel workshops over the summer period and undertaken multiple prioritisation exercises within the multi-disciplinary research team. The resultant intervention ideas centre on promoting the acceptability of accessing psychological support and organisational support. Accordingly, the research team have been working on generating and progressing ideas for interventions to meet this aim.
The approach used to develop interventions in a short period of time has been written up and published.
Gibson Smith K, Cunningham K, Cecil J, Laidlaw A, Cairns P, Scanlan G, Tooman T, Aitken G, Ferguson J, Gordon L, Pope L, Johnston P, Wakeling J & Walker K. (2021) Supporting doctors’ wellbeing and resilience during COVID-19: A framework for rapid and rigorous intervention development. Appl. Psychol.: Health & Wellbeing. 10.1111/aphw.12300
Initially we took forward five interventions to promote accessibility to informal and formal psychological support.
Wellbeing website
Participants identified that is would be helpful for the availability of resources to be kept in one place that would be easy to access, for example, a website. The project team identified that a website (PRoMIS www.promis.scot) had recently been made publicly available to all health and social care professionals. Therefore, we collaborated with the website managers to use our emerging evidence to provide further information and help to develop it further.
Composite narrative animations
Narratives are stories which include characters and linked events which can portray beliefs, intentions and behaviour. Composite narratives are narratives designed from the multiple experiences of a sample and can add an authenticity to a narrative. Video based narratives or animations can be significant drivers of attitudinal and intention changes. Therefore, we have utilised the evidence base provided by the data collected during the study with the Behaviour Change Wheel (BCW), a framework for intervention development based upon the Capability, Opportunity, Motivation – Behaviour (COM-B) model of behaviour change to develop animations aiming to enhance the acceptability of doctors seeking formal and informal psychological support. The use of the animation and our evidence ensures that they are credible and highlight authentic experiences. It was decided to develop an animation derived from data for each of the following groups: GPs, Foundation doctors, early year specialty trainees, later years specialty trainees, and senior hospital doctors using a professional animation company.
Jane, the GP (as seen below) was the first one to be developed. This was shown to our participants during the final interview to ascertain their views. It was well received with many helpful comments regarding their future development. It is hoped to update Jane in the future.
Nadya, the junior trainee and David, the senior trainee are currently in development, funded by NHS Education for Scotland. It is anticipated that they will be ready for release by the end of the year.
Bryony, the senior doctor animation is due to be developed early in 2022 with the support of NHS Grampian where it will be piloted as part of the “we care” programme to support doctors wellbeing.
At the present time, we are actively seeking funding for Hamish, the foundation trainee to support foundation doctors in their wellbeing.
Wellbeing spaces
To encourage boards to consider reintroducing/enhancing/signposting hospital R&R wellbeing spaces, we produced a persuasion document that outlines the benefits that these spaces offer in terms of wellbeing and the organisational commitment to staff wellbeing and an infographic (see below).
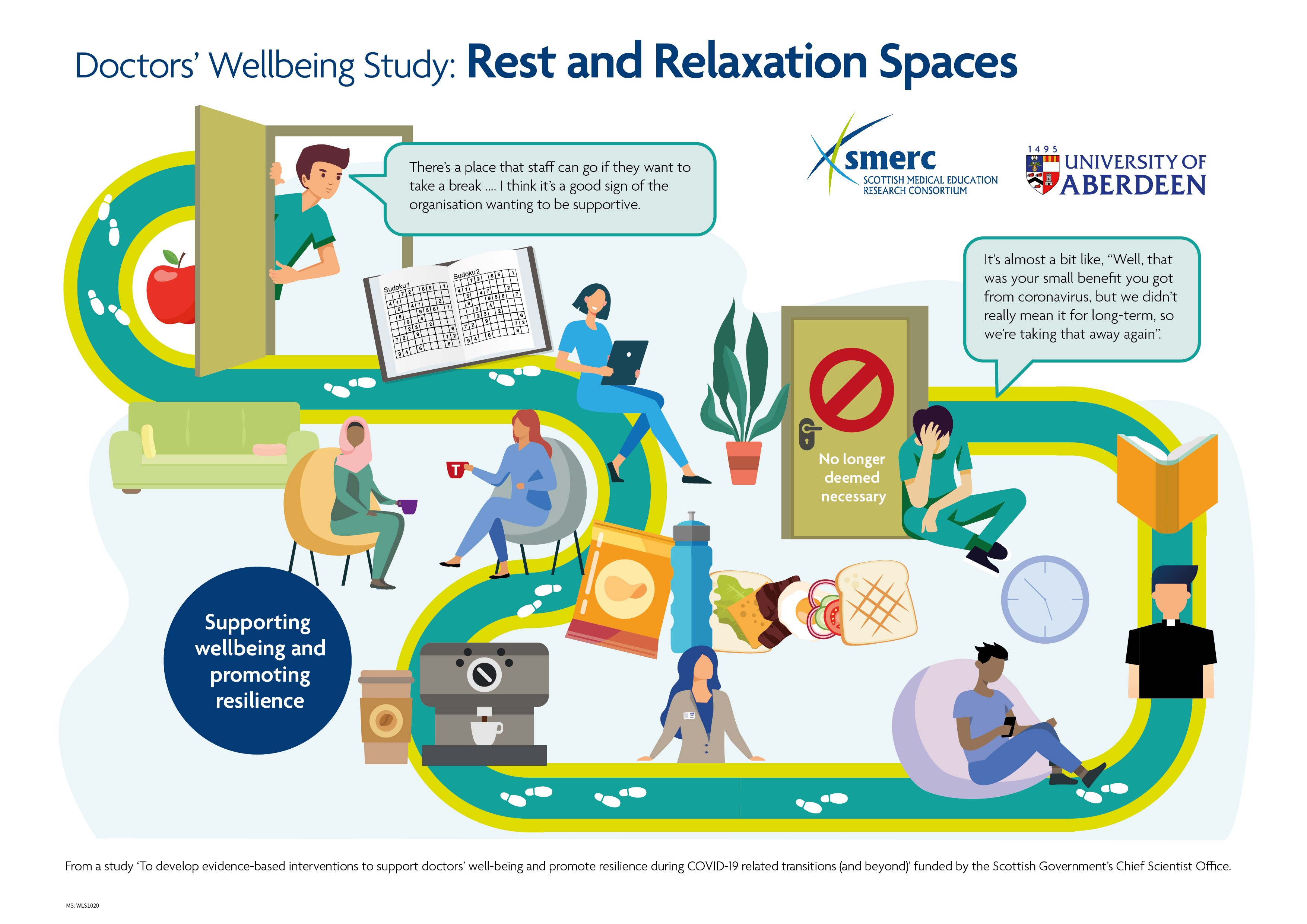
This document has been sent to NHS Boards emphasising the importance of these spaces and highlighting where staff can readily access them. We asked our participants about R&R spaces during the final interview. We also collected additional data from all the NHS Boards in Scotland on their current and specific R&R provisions. It has become apparent there are some differences in perception relating to what the Board consider is available and accessibility and what staff consider is available and accessible.
A paper is being prepared for publication.
Informal in-person support
To encourage doctors to access wellbeing support, we were looking to develop an intervention to provide informal in-person support. Our intervention would involve retired doctors and psychologists (on a voluntary basis) trained to provide wellbeing support to doctors within an R&R space. Informal one-to-one support, informal support to groups (face-to-face or online), active signposting to wellbeing resources and referral to formal psychological support would hopefully be offered. Unfortunately, for a several reasons, this intervention was unable to be completed. However, we are pleased to note that informal in-person support is now being provided in some of the NHS Boards.
‘How was your day?’ app
We have collaborated with NHS Lothian, NHS Tayside and the company Trickle 'How was your day?' Trickle app to develop an additional component to their employee and wellbeing app which gives individuals a simple way to monitor their personal sentiment and understand the reasons for driving it whilst providing insights at an organisational level that reveal how people are feeling so pro-active support cant be facilitated. The additional part to the app takes a proactive approach to supporting and valuing staff prompting them each day with the question “How was your day (HWYD)?”. Responses are recorded together with factors that affected their day. Feedback is then provided on what made mostly positive days and/or negative days with some suggestions as to how to make the negative more positive and what makes them have a positive day. The app was launched in December. Since then, further developments have been implemented, for example, the icons representing reasons for affecting their wellbeing have been updated and revised following user feedback, information provided to both the user and the organisation has become more detailed together with more instant feedback.
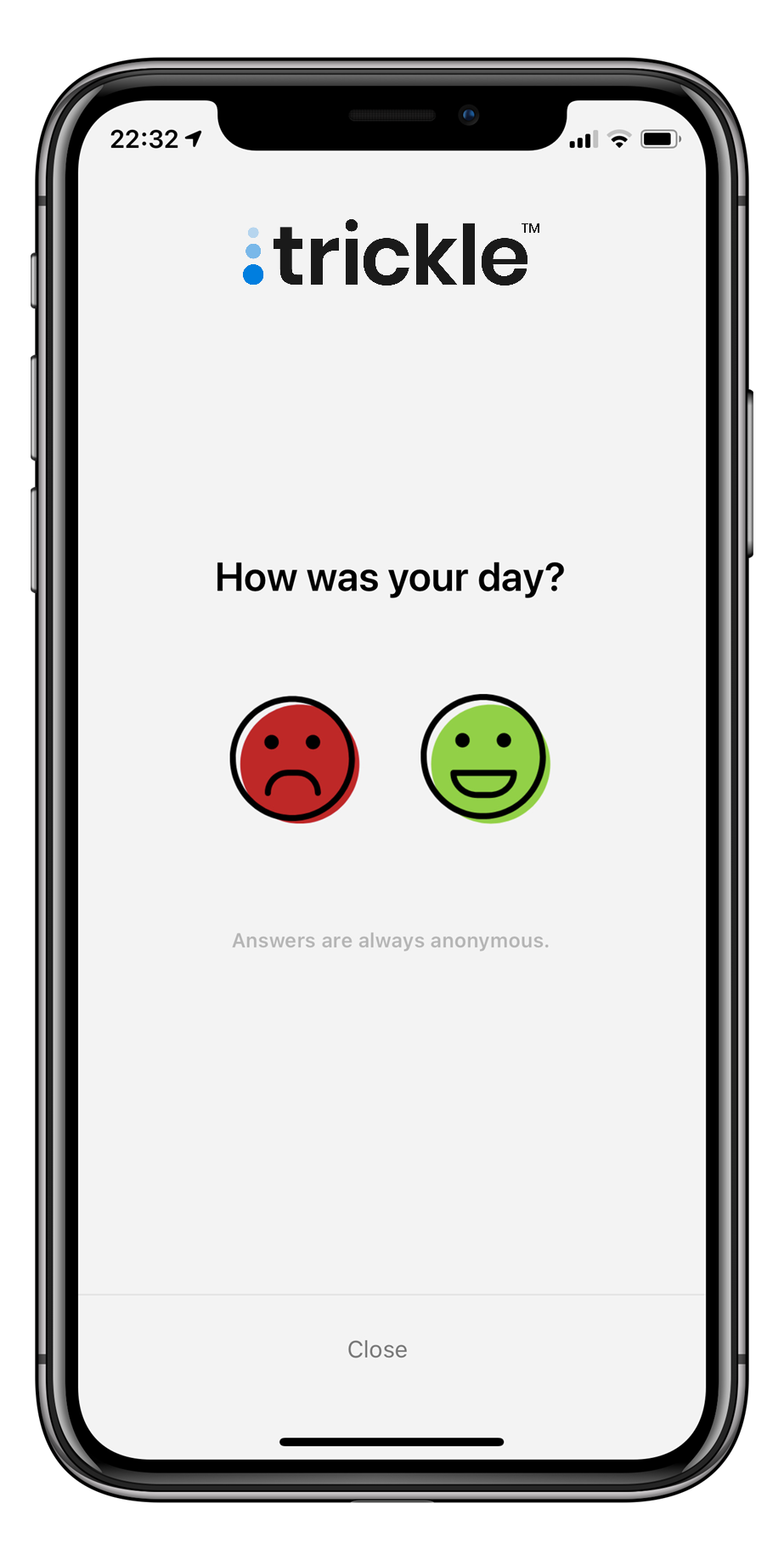
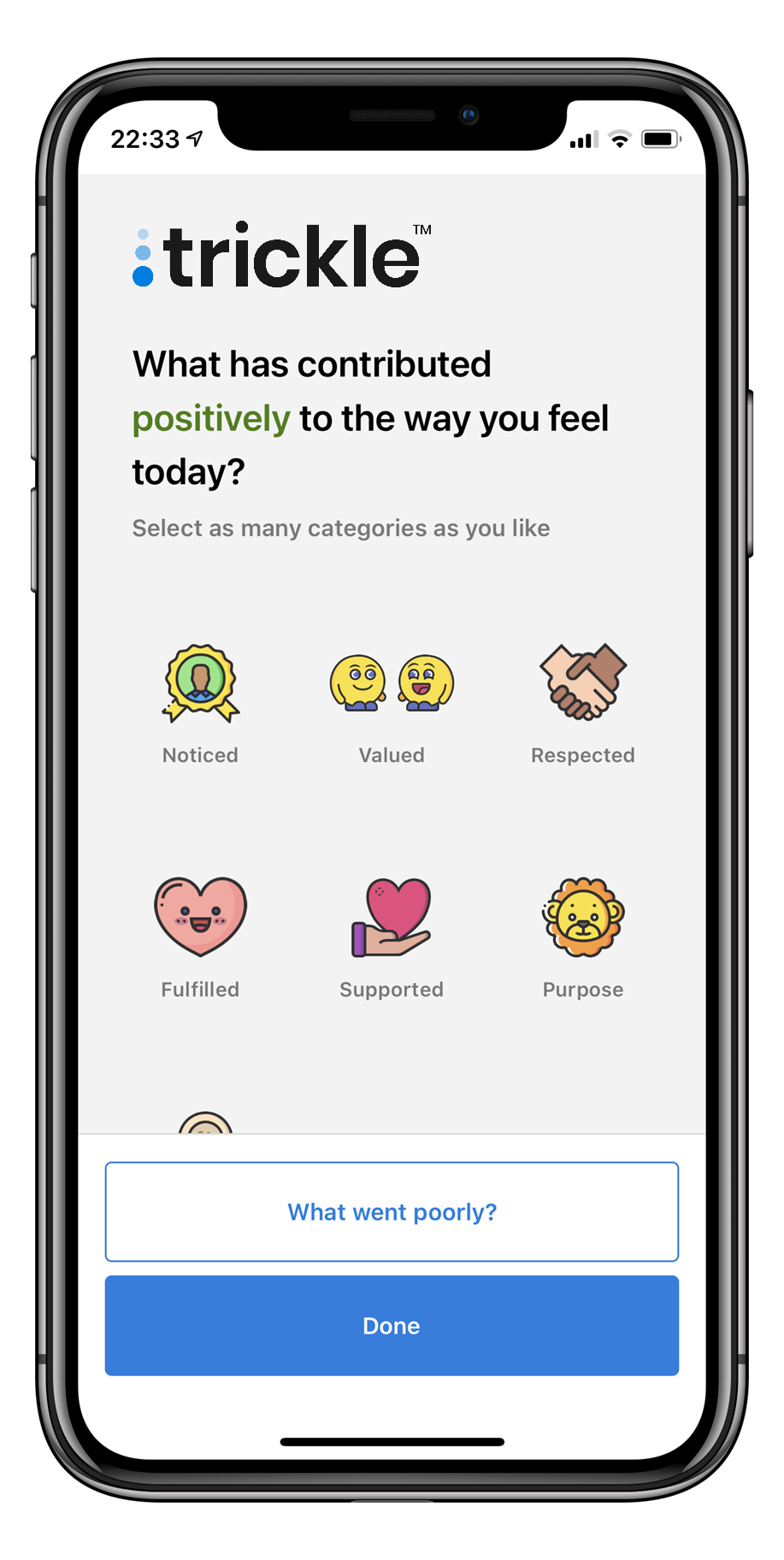
The HWYD part of the Trickle works app is now used by many healthcare organisations and has been cited as the reason for using the app within the organisation to ensure that the organisation has oversight of the wellbeing of its staff and how to support them.
A paper is being prepared for publication.
Workstream 4 - Evaluation
Participants have initially evaluated the interventions positively. Doctors have indicated that they feel heard through participation in this study and are supportive of the interventions that have been prioritised. Doctors at different stages of their career require different types of support and our research indicates that multiple interventions are required. All our partners in the various interventions will be undertaking a longer-term evaluation in conjunction with the research team.
Initial key findings
The pandemic has magnified existing challenges to healthcare staff wellbeing.
What they want to be and feel is :
Did you know?

Other publications:
Johnston P (on behalf of SMERC project team). Keep calm and carry on – but what is being done to look after doctors during COVID-19 and beyond? BMJ March 2021
The future
We have conducted 3rd interviews with our participants and are currently working on the analysis of the data. An application is currently underway for more secondary analysis. The title of our future projects will be linked to the three key words that underline what the doctors told us: Heard, Valued and Supported.
Contact details
Please feel free to contact the Principal Investigator of the project, Dr Kim Walker (kim.walker@abdn.ac.uk), if you have any questions, would like to request further details of the study or to discuss future collaborative projects where our evidence may be of benefit.
This page was last updated on: 07.12.2021 at 14.55